

Health facilities providing comprehensive emergency obstetric and newborn care services including deliveries by Caesarean section (C-section) surgery and blood transfusion services are designated as First Referral Units (FRUs) in India. The FRUs have doctors trained in obstetric surgery, anesthesia and specialist paediatric care as well as nurses specially trained to identify and manage most complications of pregnancy. They have fully equipped Operation Theatres (OTs), emergency and recovery wards and labour rooms with the requisite medical supplies and equipment and blood transfusion supplies. These FRUs provide all the defined nine signal functions that are included under Comprehensive Emergency Obstetric and Newborn Care (CEmONC). Government of India, in its Maternal and Newborn Health Toolkit, recommends that, there should be at least one FRU for every half a million population, geographically well distributed within each district, to ensure easy and timely access to CEmONC services1.
Nine Signal Functions (SFs) form the basis for considering a health facility to be providing CEmONC services and functioning as an FRU:
SF 1: Administration of Antibiotics
SF 2: Administration of Oxytocic Drugs
SF 3: Administration of Anticonvulsants
SF 4: Manual Removal of Placenta
SF 5: Removal of Placental Remnants
SF 6: Assisted Vaginal Delivery
SF 7: Newborn Care and Newborn Resuscitation
SF 8: Caesarean Sections
SF 9: Blood Transfusion services
First Referral Units (FRUs) are required to be equipped with a specialized workforce that can manage all the major medical causes of maternal and neonatal deaths. Hence, adequate number and distribution of active FRUs is imperative for
preventing and reducing the high maternal mortality ratio in Uttar Pradesh (UP). Timely and good quality emergency obstetric services will also have a major impact in reducing neonatal mortality rates in UP. A significant barrier in activating FRUs in UP is the paucity of specialist doctors in the government health services. With only 221 Anesthetists and 198 Gynecologists working as a part of Provincial Medical Health Services cadre, the State has more than 80% vacancy in these two specialist posts, as of 20182. In addition to this, there is lack of critical equipment or infrastructure essential for a functional operating theatre. Multiple initiatives as short, medium and long term measures have been undertaken to address these barriers for FRUs by the Government of UP (GoUP).
This initiative incorporates policy enablers for posting and leveraging available MBBS government medical officers trained either in Emergency Obstetrics (EmOC) or in Life Saving Anesthesia Skills (LSAS), as a pair with complementary skills that are required to conduct C-section deliveries at inactive FRUs (Figure 1).
The policy enablers include the opportunity of six months of clinical mentoring in obstetrics or anesthesia at the District Hospital (DH) under specialist guidance, along with the provision of incentives for C-sections conducted at the inactive Community Health Centre (CHC)-FRU. Further, there was a legal indemnity cover provided by the government (GoUP) to the EmOC-LSAS doctors for any legal damages for complications arising from the conduct of C-sections. The Model was initiated by a transparent ‘Open Counselling’ session of EmOC-LSAS doctors for selection of inactive FRUs in the presence of state government authorities in February 2019 and September 2019, referred as Buddy Buddy 1 and Buddy Buddy 2 batches respectively. The medical officers were called in order of seniority of service during the counselling process, to select the inactive FRUs where they would prefer to be posted.
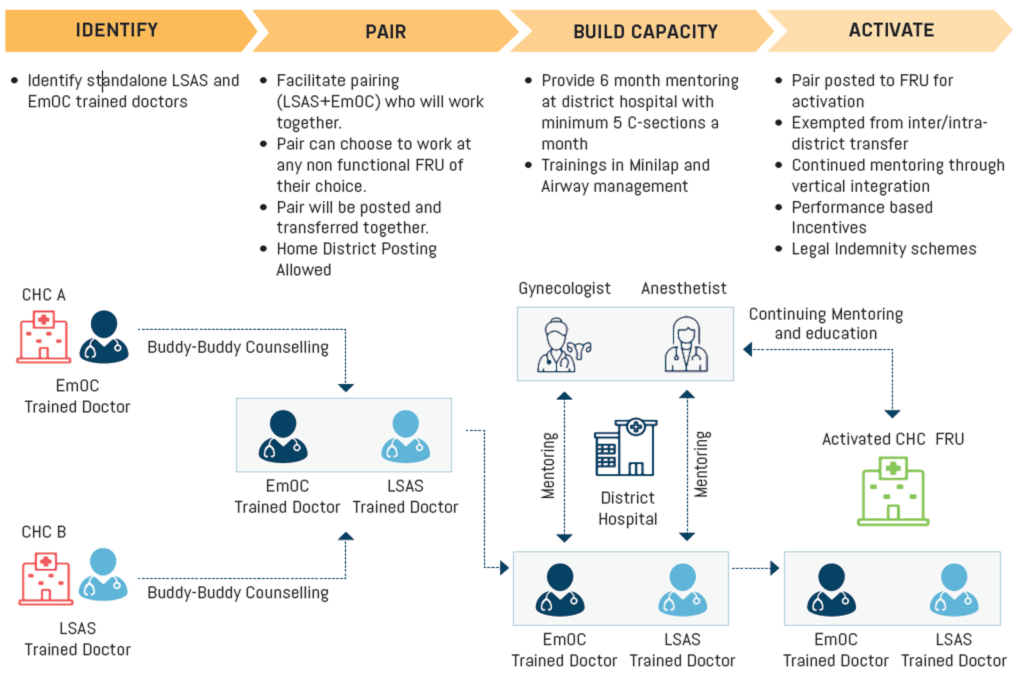
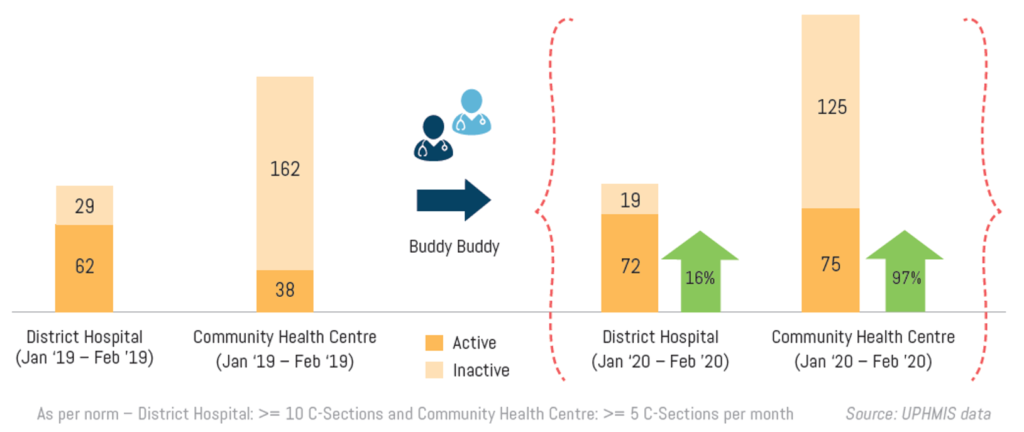
Figure 2 shows the significant increase in the number of FRUs activated during the period of one year, beginning from February 2019, when first counselling of Buddy Buddy pair doctors was conducted, to February 2020. The number of CHC-FRUs conducting C-sections increased from 38 FRUs to 75 FRUs, which is a remarkable 97 percent increase in active CHC-FRUs in a period of one year. In addition, there was an increase in the number of active DHs from 62 to 72 DHs – a 16% increase.
The Government of India recognized the Buddy Buddy Model for rapid activation of First Referral Units at the ‘National Summit on Innovations and Best Practice’, held in Gandhinagar, Gujarat in December 2019.

The progress indicates that the Buddy Buddy Model can be considered as a key approach for activating the FRUs in a short period of time. GoUP with support from UP TSU plans to accelerate the process of accreditation of more medical colleges as LSAS and EmOC training centres in order to increase the pool of MBBS trained doctors every year in this regard. Due to the sustainability and policy decisions of 2020, 48 FRUs can potentially be activated every year, however there is scope to expand upon this number significantly over the next 2-3 years. In addition, GoUP also provided an additional incentive for career progression to doctors choosing to undergoing EmOC-LSAS trainings and activating inactive FRUs. In early 2020, GoUP revised its policy pertaining to awarding additional weightage of marks for in-service candidates (regular cadre doctors serving in government facilities) for National Eligibility Cum Entrance Test (NEET) Post Graduation examination. On the basis of this policy, additional marks will be awarded in a differential manner for each year of services depending on the location of the particular health facility. However, EmOC-LSAS trained doctors who are providing CEmONC services at FRUs may be eligible for higher additional weightage as compared to other in-service doctors for serving in the same geography.
All these efforts along with creation of “specialist cadre” has the potential to ensure availability of adequate specialists at all designated 305 FRUs within next 2-3 years. Subsequently, GoUP can start planning towards designating additional FRUs and ensuring specialists availability at those so that the state can achieve the goal of having FRUs as per the population norms for FRU availability.
Kirawali CHC is one of the designated FRUs in Agra, which was inactive until the Buddy Buddy Model was implemented. Dr Anjana Singh and Dr Ajay Garg are highly motivated professionals working in Kirawali CHC. Together, they have conducted more than 50 C-sections till December 2020 in their facility.

“I was trained on EmOC about 5 to 6 years ago; however, I never got any hands-on mentoring for the same and I couldn’t practice what I was trained for. After the Buddy Buddy Model was introduced, I could choose to be posted at Kirawali CHC, Agra, which is around 20 Kms from my residence; which further made it possible for me to attend to emergency cases at odd hours. Throughout my tenure here, I have received full support of all the UP TSU team members in all technical gaps that I had shared.
was privileged to conduct a successful C-section, with support from my Buddy Dr. Ajay Garg, on the very first day of my posting here and still the glimpse of the happy mother with her healthy new born, lingers in my heart”.
“I was invited for the Buddy Buddy Counseling in 2019 and was given the opportunity to select the FRU and the Buddy of my choice. According to me, the Buddy Buddy Model is a great initiative to upskill the LSAS and EmOC specialists and provide them the platform to conduct C-sections confidently. About 8 to 9 years back, I had received the LSAS training and being posted at a Primary Health Centre, I did not get any opportunity to put to practice what I had always envisioned for. But, as it is said, better late than never, through the Buddy Buddy intervention, I not only got the training and mentoring for LSAS, but I could also successfully support conduct of C-sections right
from the day one of my posting at Kirawali CHC (FRU). The successful conduct of C-sections was much appreciated in the District Health Society Meeting”.

2Manav Sampada, Government of Uttar Pradesh’s Human Resource Management System, 2018